MGUH Pediatric Radiology Home Page
Welcome!
This website was designed to provide useful resources for your residency training in pediatric radiology. Please bookmark this website and refer to it as you rotate through pediatric radiology. You might also find these resources useful for call.
As a reminder, each resident will have 3 rotations in pediatric radiology:
- 1st rotation @ MGUH, Resident Year 1 (PGY-2)
- 2nd rotation @ CNMC, Resident Year 2 (PGY-3)
- 3rd rotation @ CNMC, Resident Year 3 (PGY-4)
Resident Quiz
Each resident is required to take a pre- and post-rotation quiz during their 1st rotation on peds. This quiz is designed for 1st year residents (junior level). It contains 60 questions which you must complete in 60 minutes. Please use the link below to launch the custom test interface and start your quiz.
Senior residents have the opportunity to take a mock board exam. This exam uses the same custom test interface and covers a greater breadth and depth of pediatric radiology. The questions are more difficult and there are roughly 185 questions. You will have 3.5 hours for the mock board exam.
Please treat these quizzes as though you were taking a formal board exam. Take these quizzes in exam-like conditions that allow you to concentrate. Do not discuss the test questions with your peers and please do not distribute the questions to others.
When you are ready, click the link below to begin your quiz.
Educational Cases
Click below to select a case to review.
<< (1) (2) (3) (4) (5) (6) (7) (8) (9) (10) >> NEXTmyPEDRAD
myPEDRAD is now LIVE! Each resident will have access to an individual dashboard keeping track of your progress towards completion of training in pediatric radiology. You will be able to review exam scores, rotation feedback, and your resident passport.
Your username and password will be assigned to you. These cannot be changed. A link will be provided to send you an email reminder if you forget your login credentials.
Administrator access is granted to the program directors (Ann Jay and Danielle Demulder) and course directors (Rocky Zandieh and Christabel Lee).
Basic Web Course
IN PROGRESS
I am making progress in completing a basic, introductory web course. All student learners should take the course as an independent learning experience. The material is very basic, designed specifically for junior residents and medical students. Please visit the site and go through the completed sections. The following weblink will launch the site for you:
Journal Club
How Journal Club is run:
We will have a pediatric journal club during noon conference two times each year. Article assignments will be made for every resident to read to prepare for these conferences. You can download the articles from this website. A reminder email will be sent to you a few days before the journal club.
The articles will have a common topic and we will review them in a round-table discussion, led by a team of THREE 1st year residents according to the assignments below. Each 1st year resident will share responsibility with their classmates for 1 journal club conference, each year.
Upcoming Journal Club:
RED TEAM Resident Assignment:
- Emily Rutan
- Kim Nguyen
- Haley Swanson
Date: TBD - ETA Nov. 2019
Articles:
- Testicular torsion with preserved flow: key sonographic features and value-added approach to diagnosis.
Pediatr Radiol. 2018 May;48(5):735-744.
- The ultrasonographic "whirlpool sign" in testicular torsion: valuable tool or waste of valuable time? A systematic review and meta-analysis.
Emerg Radiol. 2018 Jun;25(3):281-292
- Ultrasonography of Extravaginal Testicular Torsion in Neonates.
Pol J Radiol. 2016 Oct 1;81:469-472
- Ultrasonographic Assessment of Testicular Viability Using Heterogeneity Levels in Torsed Testicles.
J Urol. 2017 Mar;197(3 Pt 2):925-930
Previous Journal Club Sessions & Topics
N/A.
Suggested Reading for Rotations and Boards
Textbooks
You will find that every subspecialty in radiology has a monstrous, intimidating book with thousands of pages and countless figures, tables, references, and chapters... chapters upon chapters... As a resident, I am sure you appreciate being told to read these books -- and by all means, if you are able to do so, please do. In pediatric radiology, that book is Caffey's.
As a more realistic expectation, I would like you to read Donnelly's Fundamentals of Pediatric Radiology. This is a great overview, it is well-written and a light-weight read.
The next step up is the Pediatric Radiology Requisites, recently updated by Michele Walters and Richard Robertson. This is a fantastic textbook and is my second recommendation for formal textbook reading, after you finish Donnelly.
Last but not least, the Caffey book is the definitive textbook reference, but this is not a requirement so much as a suggested read.
 Fundamentals of Pediatric Radiology Lane Donnelly |
 Pediatric Radiology: The Requisites M. Walters & R. Robertson |
 Caffey's Pediatric Radiology Brian D. Coley (2 volume set) |
Cases & Review books
These type of books are great to read but do not necessarily provide the groundwork for a solid foundation in your knowledge base. They are really designed more for board preparation and to supplement your fundamental learning, which hopefully you will build through your rotations, lectures, and your own independent reading. Among the case-review books, here are the resources I recommend:
 Case Review Series: Pediatric Radiology |
 Pediatric Imaging: A Core Review (Core Review series) |
 Teaching Atlas of Pediatric Imaging |
Miscellaneous Reading:
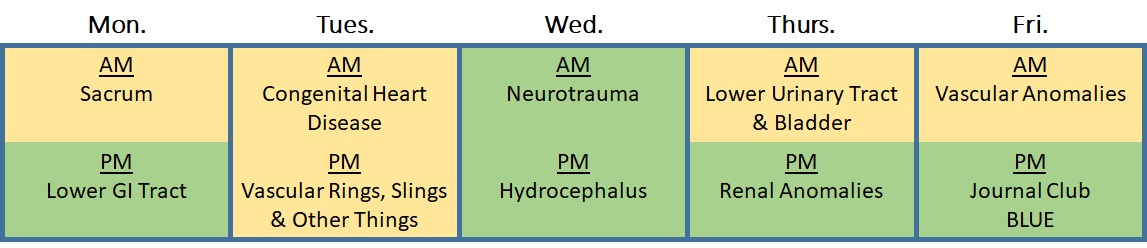
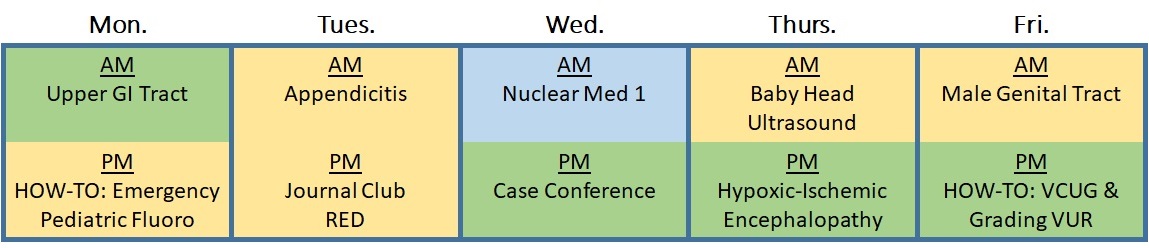
Syllabus
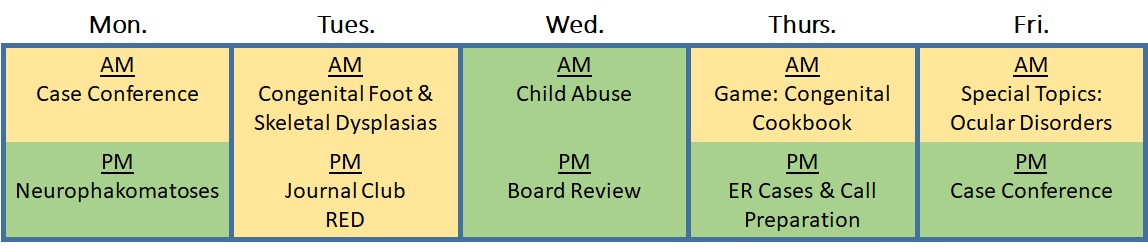
The Department is moving to a block-schedule for your resident lectures. A 2-year program has been designed to cover the spectrum of pediatric radiology expected of a general radiologist, so that you are well-equipped in your future careers. To cover this material, we will use a variety of resident conference formats: traditional didactic lectures, case conferences, interactive games, journal clubs, board review & mock boards, and practicum sessions (e.g. "How-Tos"). Please note: Journal clubs will be ASSIGNED to you. Please check the Journal Club section to check which team you are on and which articles you cover. ALL residents should prepare for journal club by reading the assigned articles
Resident Syllabus -- Pediatric Radiology
Note: We reserve the right to change course content without any advance notice.
Year 1
| Block 1 |
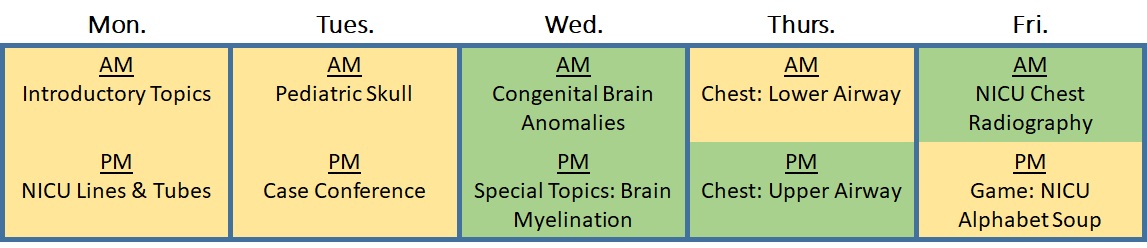
|
| Block 2 |
|
| Block 3 |
|
| Block 4 |
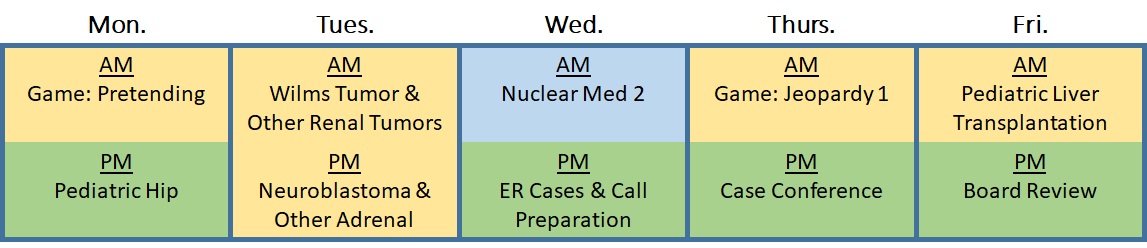
|
Year 2
| Block 5 |
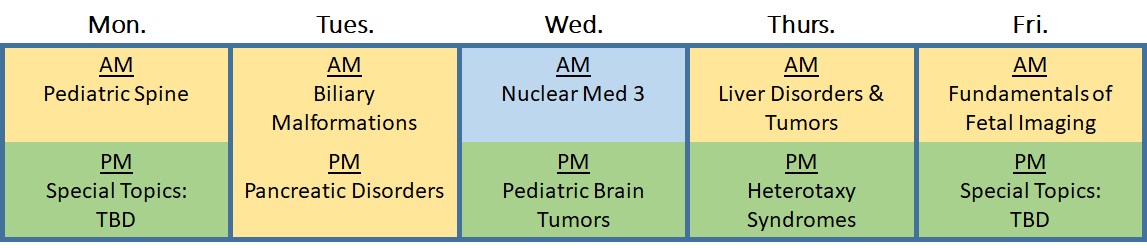
|
| Block 6 |
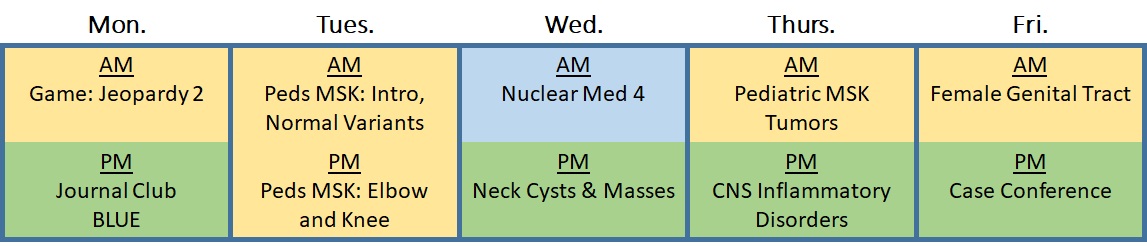
|
| Block 7 |
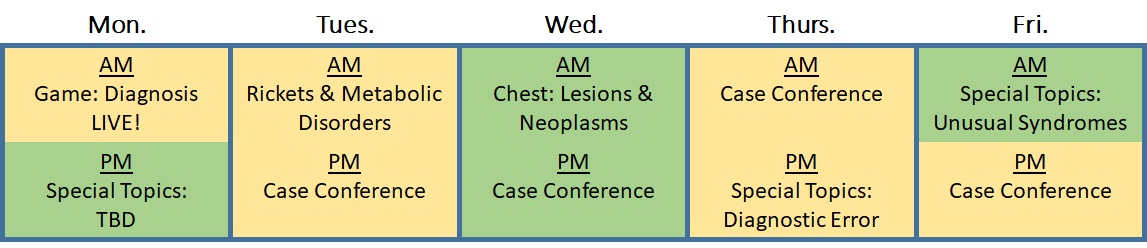
|
| Block 8 |
|
A Note about the Syllabus:
We put great effort into covering the study guide outline for the ABR Core Exam. Nevertheless, it is not possible for the resident syllabus to cover absolutely everything that can materialize on your board exams. Ultimately, it is your own responsibility to pursue independent learning and prepare for your exam. Please refer to the "Suggested Reading" section for references and review books that we recommend.
Quick Links
Useful Articles:
- Normal liver, spleen, and kidney measurements by ultrasound
- Calvarial dermoids and epidermoids in infants and children
- Urinary Tract Dilatation consensus guidelines
- Ultrasound of lumps and bumps in kids
- Bedside sonographic marking for infant LP
- Ultrasound elastography in children
- Imaging Pediatric Joints & Hips (Lurie Children's slideshow)
Useful Links
- OHSU Normal Pediatric Measurements
- Normal bones database (CNMC)
- UCSD Bone Pit -- Normal Bone reference (categorized by age and gender)
- Example normal bones of the pediatric skeleton by age
- Stanford MSK MRI Atlas
- Society for Pediatric Radiology home page
- Georgetown wiki (only accessible from MedStar campus)
- Georgetown wiki: ultrasound videos, scanning tips (only accessible from MedStar campus)
Handouts and Rotation materials
- Resident rotation passport (template)
- Resident feedback form (fillable)
- Patient certificate - MGUH
- Misc. Handout: SB cribsheet
- Misc. Handout: TB cribsheet
Policies
Table of Contents
- Attending Reads
- Same-Day Add-ons
- Chaperoned Studies
- Patient Safety
- Documenting Critical Results
- Occurrence Events and Reporting
- Skeletal Surveys
Attending Reads
Any time a physician asks you for an attending read on a pediatric patient, you should take the request seriously and act promptly. The usual scenario is for confirmation of a Dobhoff tube. When a new Dobhoff is placed, it requires some attending physician to review an xray and confirm that it terminates within or beyond the stomach. This is important even in the middle of the night, because sometimes they need to use the tube to give medications.
Occasionally the clinicians will request attending reads for other studies such as positive appy cases, stat MRI for appy, testicular or ovarian torsion, etc. Whatever the case may be, you should review the study first, make sure that image quality and protocol are appropriate, provide the preliminary interpretation, and then seek the attending read if it is still requested (or in certain scenarios, required) per discussion with the ordering clinician.
You are always welcome to reach out to me personally for any pediatric patient at night, if you are having problems reaching the assigned call attending.
Return to Top
Same-Day Add-ons
Most add-on requests will be for same-day ultrasound. Under normal circumstances, please approve same-day add-on requests from our referring pediatricians. This is especially true for our transplant patients. Any request from the Pediatric Transplant clinic should be approved. For general pediatrics, those requests should also be approved in the vast majority of cases. Some of these studies have time-sensitive constraints (spine US, hip US, baby head US all come to mind) in which ultrasound becomes limited later in development, and we don't want to contribute to this special type of limitation by having the parent(s) try to schedule an assigned appointment some 3 weeks later.
Add-on CT and xrays are straight-forward and should be easier to accommodate in our workflow.
Add-on MRI and fluoroscopy might be tricky, but if the study has any urgent implications you should make every effort to try to approve and coordinate these studies.
Return to Top
Chaperoned Studies
If the parent or legal guardian is not available, then a chaperone is mandatory for sensitive studies such as scrotal ultrasound or pelvic ultrasound. Furthermore, under no circumstances should a transvaginal ultrasound be performed in any pediatric patient without having attending radiologist approval. Transabdominal ultrasound should always be performed first and foremost. The attending radiologist who will assume responsibility for the pelvic ultrasound should provide ultimate approval for TV ultrasonography, and you should reach the attending radiologist in determining whether to perform a TV ultrasound. If this comes up at night, you are strongly encouraged to contact me directly about this.
Return to Top
Patient Safety
Patient safety is of paramount importance for us in radiology. This is especially true in pediatric radiology! In pediatrics, this means performing child-friendly studies with the radiation exposure as low as reasonably achievable (ALARA) to extract the most meaningful information.
Universal safety principles apply to our pediatric population. These include:
- observing time-out procedure and reviewing the order to verify you have the right patient and that you perform the right study prior to any examination;
- carefully reviewing your reports to avoid any possible laterality error (left/right error);
- being mindful of potential tripping or falling hazards, especially on any surface that does not have rails (NEVER leave the child alone on a fluoroscopy table or ultrasound bed);
- double-checking any patient allergies prior to giving contrast or before adding flavoring to oral contrast agents;
- observing proper hand sanitation techniques before and after any patient contact;
- and observing any isolation precautions to avoid transmission of infectious agents among our pediatric populations. Remember that enteric precautions (which are fairly rampant among our patients) require vigorous hand-washing with soap and water.
If you have any saftey concerns whatsoever for any pediatric patient, you should feel comfortable contacting an attending to express your concern or ask any question you may have. You are always welcome to contact me regarding these issues and I would like to be notified of any patient safety issues that occur for any of our pediatric patients.
Return to Top
Documenting Critical Results
Please abide by the department policy regarding documentation of critical values. Use the "Powerscribe Critical" template and be sure to indicate when you recognized the critical finding, who you spoke with including first and last name (must be an MD, NP, or PA), method of communication, and time/date of communication.
Return to Top
Occurrence Events and Reporting
Please be sure to document any occurrence events (e.g. extravasation events, contrast reactions, falls, wrong site/wrong procedure red flags etc.), especially during call shifts. Use the electronic reporting system. You are encouraged to report anything and everything, according to your judgment.
Return to Top
Skeletal Surveys for Suspected NAI
Please contact me immediately for any case of suspected child abuse. These cases require the oversight of an attending physician. A skeletal survey should not be performed without the input of the supervising attending. I strongly believe the patient should be kept in the xray exam room while the images are carefully reviewed to make sure all the needed views are obtained prior to releasing the patient from the department.
Refer to the "Protocols & Procedures" section to review the recommended technique and required views for a comprehensive skeletal survey.
Return to Top
MGUH: Invited Guest Speakers in Pediatric Radiology
Grand Rounds speakers
- Sarah Bixby, MD MBA, Boston Children's Hospital
MGUH Grand Rounds Mar. 2024
Topic: The "Goldilocks" Zone in the Hip: Current Understanding and Ongoing Controversies.
Speaker profile - Eva Rubio, MD MBA, Children's National Medical Center
MGUH Grand Rounds Mar. 2023
Topic: Prenatal Imaging Features of Cloaca.
Speaker profile - Ryne Didier, MD, Children's Hospital of Philadelphia
MGUH Grand Rounds Mar. 2022
Topic: Congenital Diaphragmatic Hernia: Past, Present, Future.
Speaker profile - (HIATUS During Academic Year 2020 - 2021)
- Stephan Voss MD PhD, Boston Children's Hospital
MGUH Grand Rounds Dec. 2019
Topic: Anatomic vs. Functional Metabolic Imaging: Which is Best for Which Tumors?.
Speaker profile - Michael Callahan MD, Boston Children's Hospital
MGUH Grand Rounds Dec. 2018
Topic: Comparing the Risk of CT Ionizing Radiology and Sedation for MRI in Children.
Speaker profile - Sanjay Prabhu MBBS, Boston Children's Hospital
MGUH Grand Rounds Dec. 2017
Topic: 3D Printing and Simulation in Pediatric Radiology
Speaker profile - Arash R. Zandieh MD, MGUH Radiology
MGUH Grand Rounds Dec. 2016
Topic: Hot Topics in Pediatric Radiology
Speaker profile - Jeanne "Mei-Mei" Chow MD, Boston Children's Hospital
MGUH Grand Rounds Dec. 2015
Topic: Genitourinary Imaging in Pediatrics: State of the Art
Speaker profile
Protocols & Procedures
Overview
Several studies are unique to the pediatric population and require familiarity with proper imaging technique. These will be discussed in greater detail below. The basic protocols will be outlined and you will be provided sample images that exemplify the required views. Please note: This is NOT a comprehensive list of ALL the pediatric protocols. Furthermore, many times the adult protocols can be extrapolated to the pediatric patient with few modifications (e.g. Ultrasound liver transplant protocol, Ultrasound Abdomen Complete, etc.)Table of Contents
- Ultrasound Protocols -- VIEW ALL IN PDF
- US: Infant Spine
- US: Intussusception
- US: Pyloric Stenosis
- US: Head Ultrasound
- US: Pediatric Appendicitis
- US: Pediatric Neck
- US: Infant Hip (r/o DDH)
- US: Child Hip (r/o hip effusion)
- CT Protocols
- MRI Protocols
- Fluoroscopic Procedures
- Air Reduction Enema for Intussusception
- Voiding Cystourethrogram
- Pediatric upper GI Series
- Contrast Enema
- Airway Study
- Skeletal Survey for Suspected NAI
- Guidelines for Contrast Agent Selection
Ultrasound Infant Spine
Probe selection: ML6-15, L9, L11
Typical age group: Newborn up to roughly 4 months of age. Older is limited.
Sequences:
- Single high-quality sagittal panoramic view (LOGIQview) lumbar and sacral spine
- Sag cine sweep from sacrum through lumbar spine to cover conus (allows for counting)
- Sag cine with probe held still to check nerve root pulsation in cauda equina
- Transverse sweep lumbar spine through sacral spine (eval of posterior elements)
- Targeted sag and transverse images of area of sacral dimple, tuft of hair, or other area
- *Bilateral kidney survey: sag and transverse images of both kidneys
Return to Top
Ultrasound Intussusception
Probe selection: ML6-15, L9, C2-C9 (depending on patient size)
Typical age group: 3 months to 3 years. We will offer scan at any age requested.
Sequences:
- Targeted US of RLQ in transverse and sag plane
- Transverse cine sweep through right lower quadrant
- Color Doppler images if an intussusception is discovered
- Measure max AP diameter in transverse plane if an intussusception is discovered
- 4 quadrant survey of abdomen
- *Bilateral kidney survey: sag and transverse images of both kidneys
Return to Top
Ultrasound Pyloric Stenosis
Probe selection: ML6-15, L9, L11 (depending on patient size)
Typical age group: 1 months to 2 months. We will offer scan at any age requested.
Sequences:
- Targeted US of pylorus; show pylorus in longitudinal orientation
- Measure pyloric wall thickness (hypoechoic section)
- Measure pyloric channel length
- Cine loop with probe held still to see if there is passage of fluid or air
- Cine loop while the infant is feeding, focus on pylorus, see if milk / formula goes through
- Transverse sweep SMA / SMV relationship images in color Doppler and grayscale
- *Bilateral kidney survey: sag and transverse images of both kidneys
Return to Top
Ultrasound Head
Probe selection: C2-C9, L9
Typical age group: Newborn through 12 months; older ages become more limited (anterior fontanelle). We will offer scan if anterior fontanelle is open.
Sequences:
- Coronal still images and coronal sweep through brain using anterior fontanelle
- use both C2-C9 and L9 probes
- Sagittal still images and sagittal sweep through brain using anterior fontanelle
- use both L9 probe preferred; optimize image quality and adjust focal zones
- Sagittal midline still image
- Transmastoid views of the posterior fossa
- Spectral Doppler waveform of anterior cerebral artery in sag plane
- if requested or if there is ventriculomegaly
- Color Doppler image if choroid plexus cyst is seen
Return to Top
Ultrasound Pediatric Appendicitis
Probe selection: ML6-15, L9, C2-C9, C1-C6 (depends on patient size)
Typical age group: 4 years through 18 years. We will offer scan at any age.
Sequences:
- Targeted images of RLQ to identify appendix; provide still images and cine
- IF APPENDIX FOUND, then include:
- Transverse cine sweep of appendix from cecal base through blind-ending tip
- Sagittal cine sweep through blind-ending appendix tip
- Trans or sag cine with probe held still to show pattern of peristalsis
- Sagittal still image including appendix and cecal base
- Measure AP diameter of appendix in cross-section
- Color Doppler images of appendix in transverse and sagittal plane -- scale set to 9 cm/s or thereabouts
- Side-by-side image of appendix without and with compression
- Document if patient is tender with exam & compressions
- Document if stone is present (dependent echogenic focus with shadowing)
- IF APPENDIX IS NOT FOUND:
- Place patient decubitus to see if appendix becomes visible
- Scan before and after bladder emptying
- Obtain color Doppler image to check for regional hyperemia
- Provide one target image, label AOI, ask patient to point with 1 finger to area of pain, scan that spot
- Check for lymph nodes; if found, measure and provide at least 1 color Doppler image
- Sag image of hepatorenal space
- In GIRLS: Include both ovaries. Right ovary is most important, but try to get both. Reason: Rule out ovarian cyst, mass, or torsion as ddx.
- In BOTH girls and boys: *Bilateral kidney survey: sag and trans images of both kidneys; include color Doppler, check to rule out stones or renal pathology.
Return to Top
Ultrasound Pediatric Neck
Probe selection: L18i, ML6-15, L11, L9
Typical age group: All ages.
Sequences:
- Targeted grayscale and color Doppler of area of interest / palpable abnormality
- Contralateral views of opposite side (normal comparison)
- If lymph node or lesion is identified, give AP x TR x SI measurements
- Transverse sweep along internal jugular chain (survey for other lymph nodes)
- IF MIDLINE CYST IS SEEN
- Have patient swallow and/or stick out tongue while taking cine loop
- Label image while swallowing and hold probe still on the cyst, see if it moves
- IF MIDLINE OR PARAMEDIAN LESION IS SEEN
- Screen thyroid gland to make sure a normal thyroid is present
- IF cystic or hypoechoic structure is seen, see if structure can be compressed (? fluctuant)
Return to Top
Ultrasound Infant Hip (r/o DDH)
Probe selection: L9, L11, ML6-15
Typical age group: 4 weeks to 6 months. We will offer scan at other ages requested, but generally not > 1 year.
Sequences:
- Still sagittal grayscale image of bilateral hip
- Still transverse grayscale image of bilateral hip
- Dynamic sagittal image with stress maneuver of bilateral hip
- Dynamic transverse image with stress maneuver of bilateral hip
Return to Top
Ultrasound Child Hip (r/o hip effusion, septic hip)
Probe selection: L9, L11, ML6-15
Typical age group: Any age requested.
Sequences:
- Still sagittal grayscale image of bilateral hip
- Still sagittal color Doppler image of bilateral hip
- Cine sagittal sweep of bilateral hip
- Side-by-side comparison sagittal of both hip